News | Events
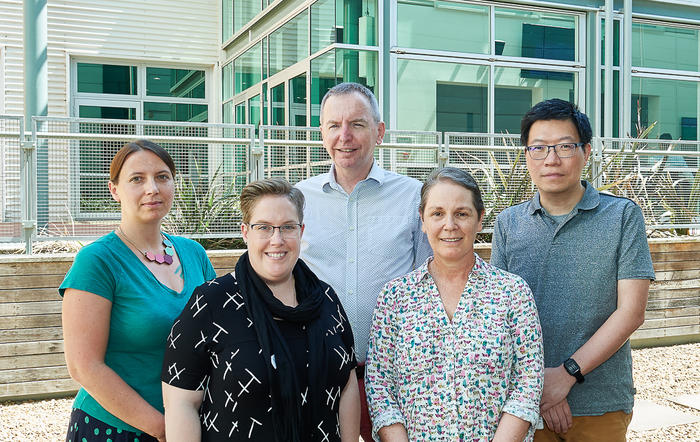
Photo: The Advanced Cellular Therapeutics Team. (L-R) Dr Federica Saletta, Ms Shiloh Middlemiss, A/Prof Geoffrey McCowage, Dr Belinda Kramer and Dr Kenneth Hsu
Children with difficult to treat bone cancer may benefit from exciting new research that shows patients' own cells may have an effective treatment.
The Advanced Cellular Therapeutics Team, at the Children’s Cancer Research Unit (CCRU), conducted the study which tested if genetically modified immune cells (called CAR T-cells) work against bone cancers.
Their aim was to inform research into effective treatments for children with bone tumours that recur or spread, such as Ewing sarcoma or osteosarcoma.
Researchers in the CCRU, the Cancer Centre for Children’s research arm, performed their results in multiple settings. These included ‘test tube’ style experiments in the lab and testing in multicellular organisms which mimic the environment that cells grow in when in people. Accomplishing significant results in these settings is a remarkable achievement.
Team members Dr Kenneth Hsu, Ms Shiloh Middlemiss, Dr Federica Saletta, Dr Stephen Gottschalk, A/Prof Geoffrey McCowage and Dr Belinda Kramer published their results this month, after peer review, in the journal Cancer Gene Therapy to add valuable new knowledge to the immunotherapy field which is just beginning to be understood.
The urgent need to provide opportunities for children with cancers that are resistant to traditional treatments was recognised by Dr Kenneth Hsu who said, “Given the limitations of current medical therapies for refractory childhood cancers, novel treatment strategies, such as CAR-T cell therapy, are highly promising.”

The CAR T-cells have been successful with other types of cancer, but little was known about if they could treat bone cancer. This study has indicated they can be effective against bone tumours which is a big step forward in developing targeted therapies for these resistant cancers.
More specifically, CAR T-cell therapy involves a chimeric antigen receptor (known as CAR), which is special receptor created in a lab that is designed to recognise specific proteins on cancer cells. This is added to a type of white blood cell, otherwise known as an immune cell, called a T-cell, to create a CAR T-cell which can launch attacks on cancer cells. Other researchers have shown that using CAR T-cells as an option is an effective way to treat patients with B cell malignancies.
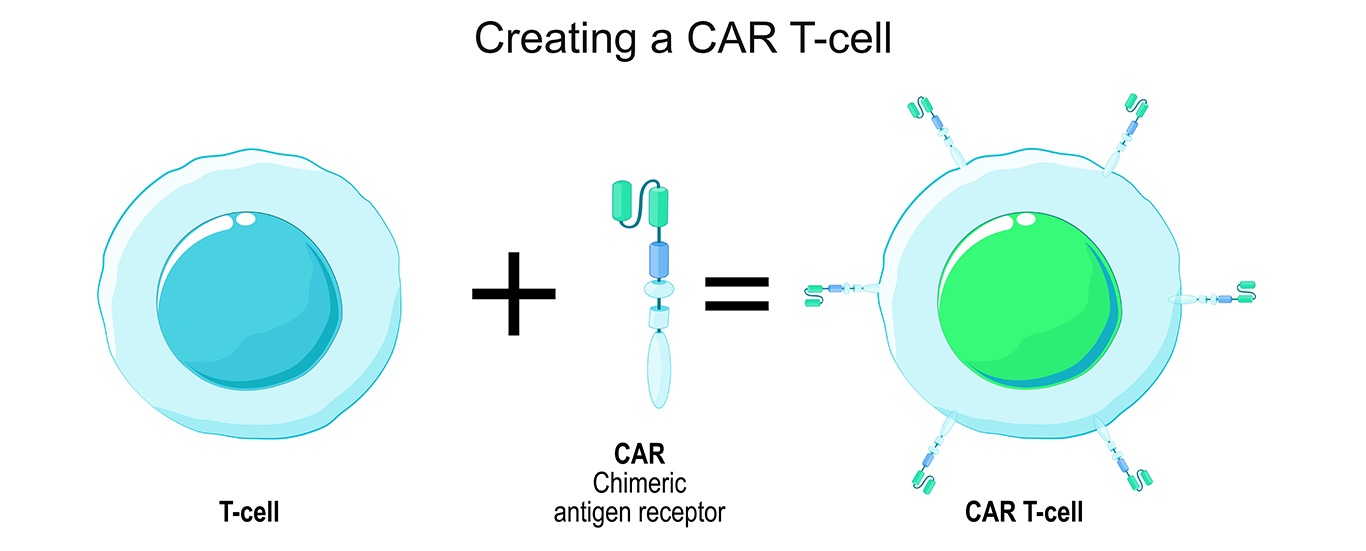
The treatment involves removing some T-cells from a patient, modifying the genes of those cells, and transfusing them back into the patient’s body. EphA2 is an antigen associated with a range of sarcomas, including Ewing sarcoma (ES) and osteosarcoma (OS) and CAR T-cells were engineered to target, latch on to, and destroy ES and OS cells. Samples of human cells were used in the tests, in a laboratory, and the impressive results of this research pave the way for future clinical developments.
Significantly, this preclinical laboratory-based research will help shape the design of early phase clinical trials which will begin the process of developing effective therapies.
The Cancer Centre for Children congratulates this team on their leadership in this vital area of research, which has yielded results of global relevance, and means we can take the next step in creating therapies that will help children with hard to treat bone tumours.
The researchers would like to acknowledge the funders The Kid’s Cancer Project (TKCP), Cancer Institute NSW through The Kid’s Cancer Alliance (KCA) and The Australian and New Zealand Sarcoma Association (ANZSA).
Read the article published in the journal Cancer Gene Therapy.